Monitoring, interventions and procedures
Checking baby's wellbeing during labour
Checking baby's wellbeing
During your labour we will recommend that you have either intermittent or continuous monitoring of your baby. It is your choice whether or not to accept this. We will recommend continuous monitoring in some situations, and for this you will need to be in a consultant-led unit.
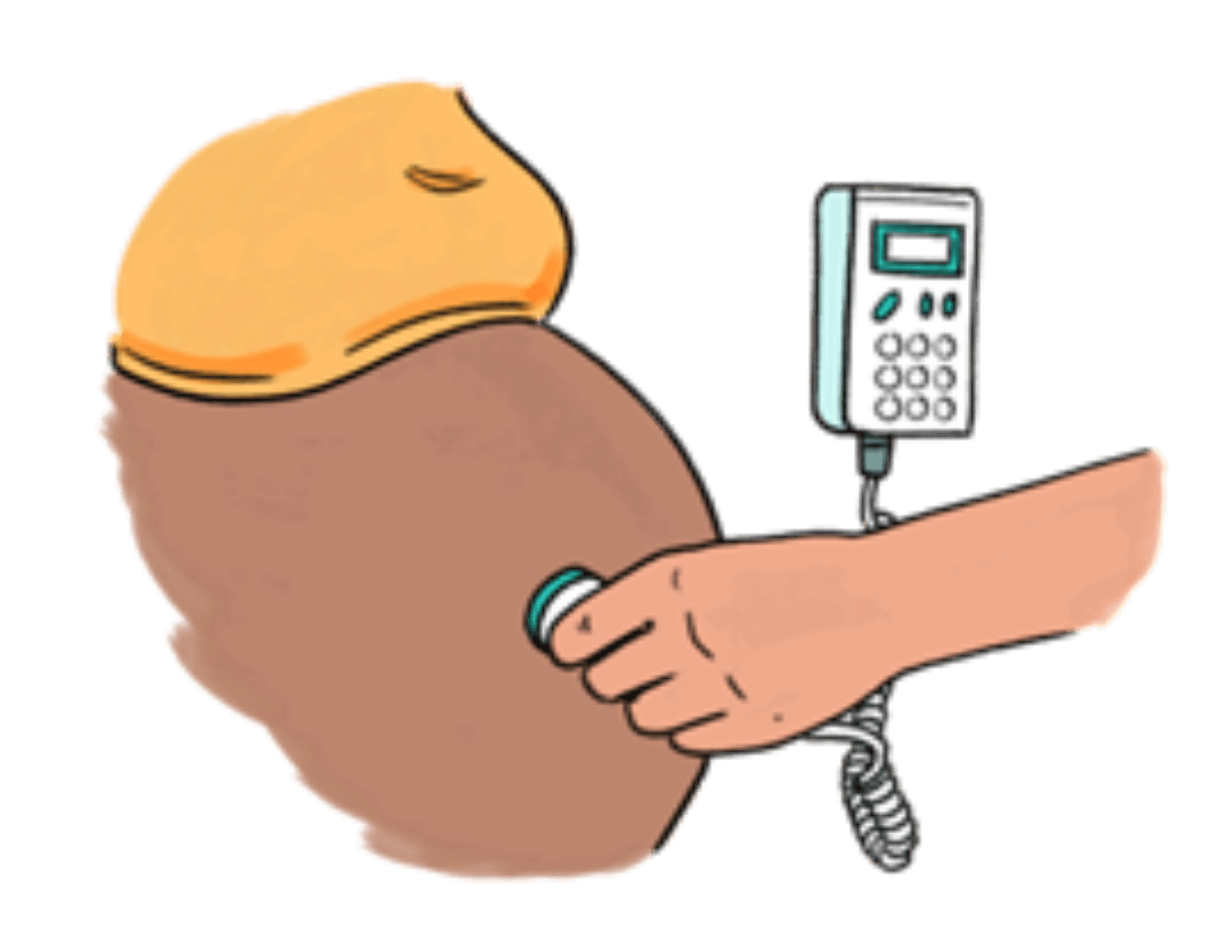
Intermittent monitoring is where your midwife will listen to your baby’s heartbeat either using a special stethoscope or using a handheld device. This is available in all birth settings.
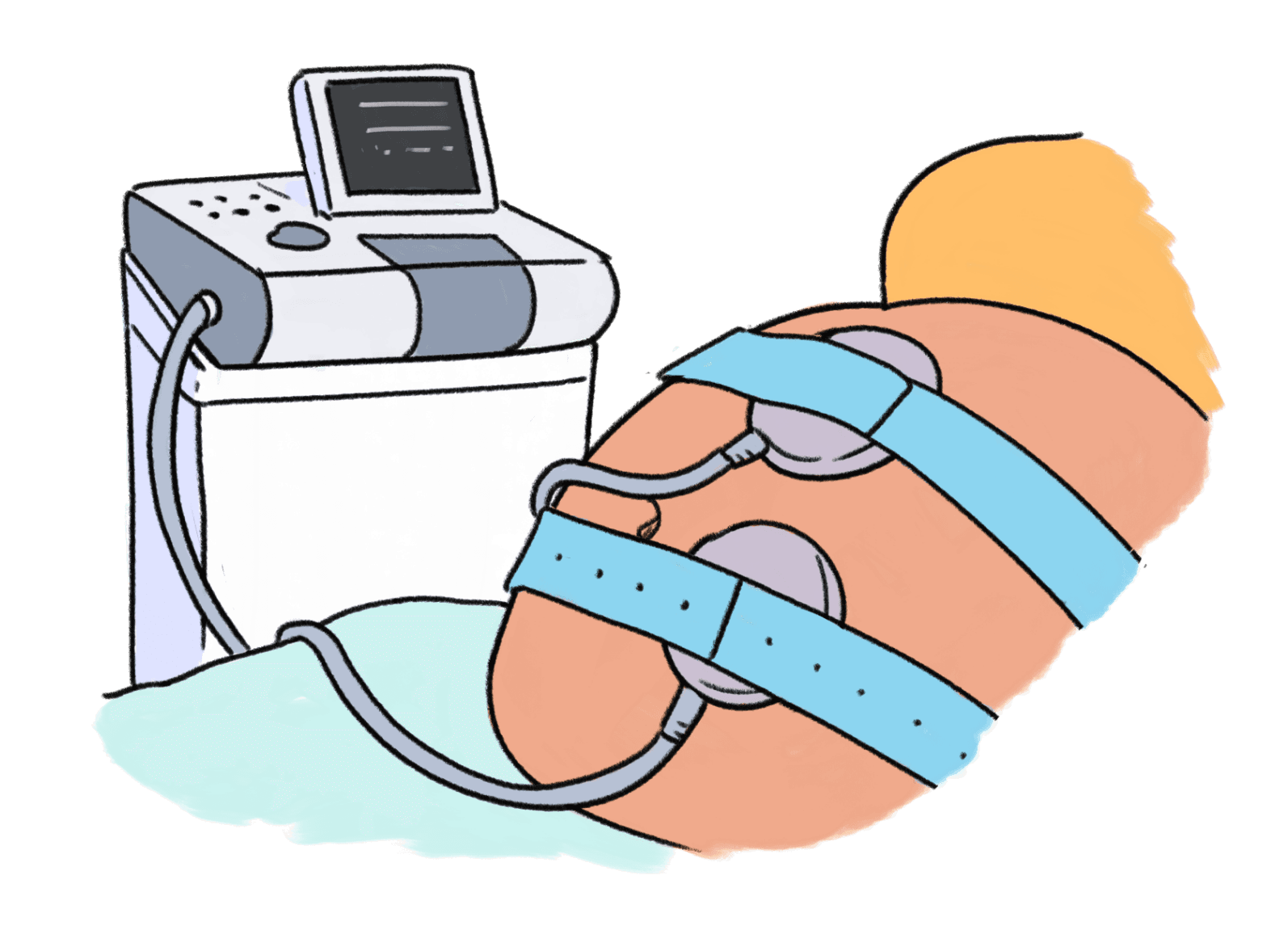
Continuous monitoring is where we monitor your baby constantly during your labour, this is called a CTG.
Cardiotocography (CTG) is a way of monitoring baby’s heartbeat and your contractions at the same time. An elastic strap is placed over your abdomen and there are two round flat parts. One of these is looking at baby’s heartbeat and the other is monitoring your contractions.
The outcomes for both of these types of monitoring are similar. The rates of cerebral palsy in babies are also the same with intermittent monitoring and CTG. Continuous monitoring is also associated with more caesarean and instrumental births. However, seizures in babies are less common when CTG is used to monitor baby’s heartbeat.
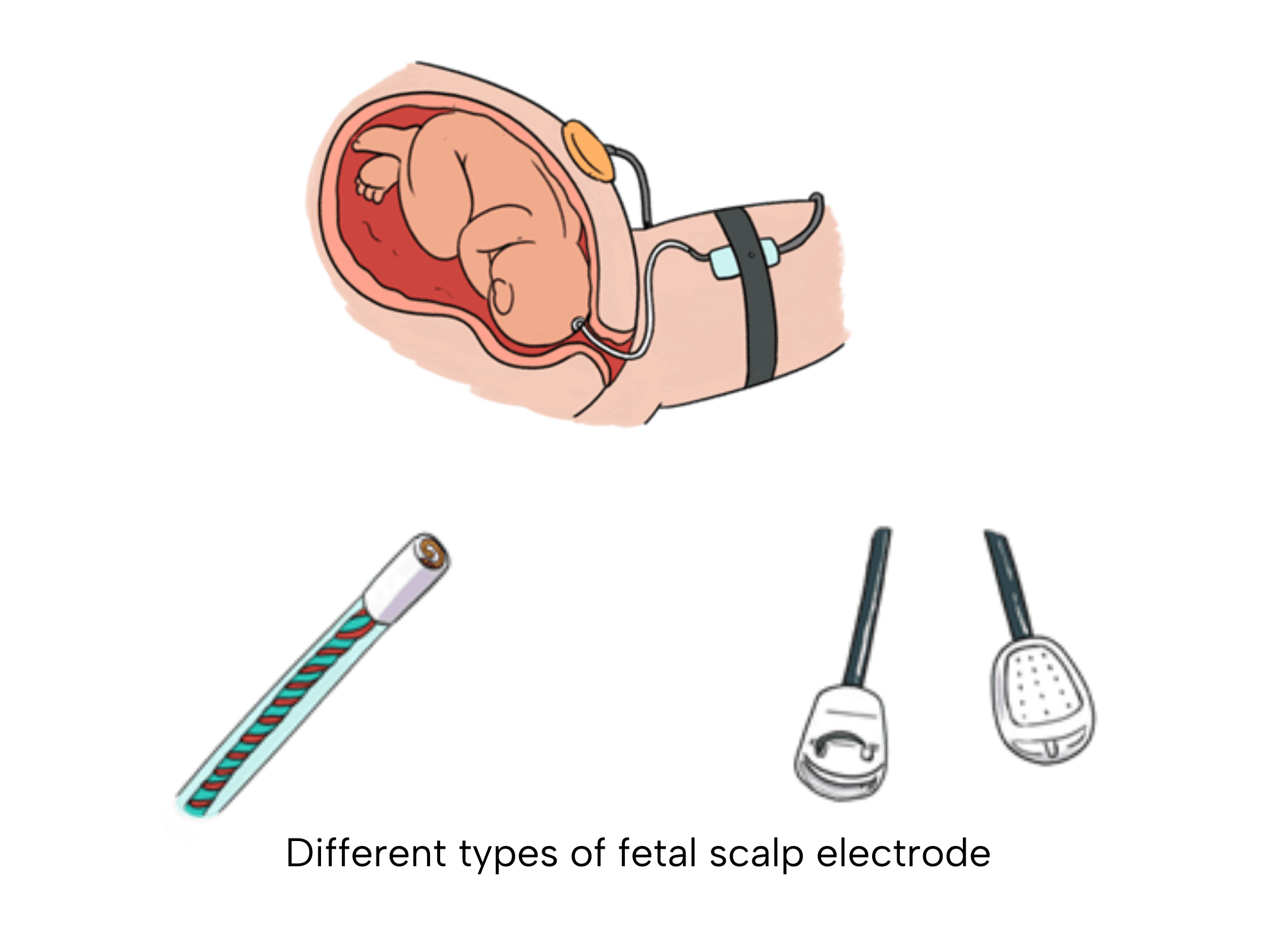
We can also continuously monitor your baby using a fetal scalp electrode. This is clip attached to baby’s head during your birth. This is a way of monitoring baby if we are unable to pick up their heartbeat through your tummy reliably. In some hospitals, the fetal scalp electrode is used routinely as part of their fetal monitoring system called ‘STAN’.
When the baby heart trace is normal, we can be sure that the baby is getting enough oxygen. When it is not normal, it is not always the case that your baby is distressed.
To try to work this out we can examine you and tickle the baby’s head. If your baby responds, we can be somewhat reassured that the baby is coping. In some circumstances, a fetal blood sample can be taken to see if your baby is getting enough oxygen. This will require you to remain still whilst a doctor takes this sample from your baby’s head. If this result is normal, it is reassuring, if it is not, we would recommend an urgent instrumental or caesarean birth.
References:
Intrapartum care. NICE guidelines Published September 29, 2023. Accessed October 18, 2023. https://www.nice.org.uk/guidance/ng235/chapter/Recommendations#planning-place-of-birth
Fetal monitoring in labour. NICE guidelines. Published December 14, 2022. Accessed October 20, 2023. https://www.nice.org.uk/guidance/ng229
Alfirevic Z, Devane D, Gyte GML, Cuthbert A. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No.: CD006066. DOI: 10.1002/14651858.CD006066.pub3