What to expect during induction
What to expect during induction
The Induction of Labour Journey
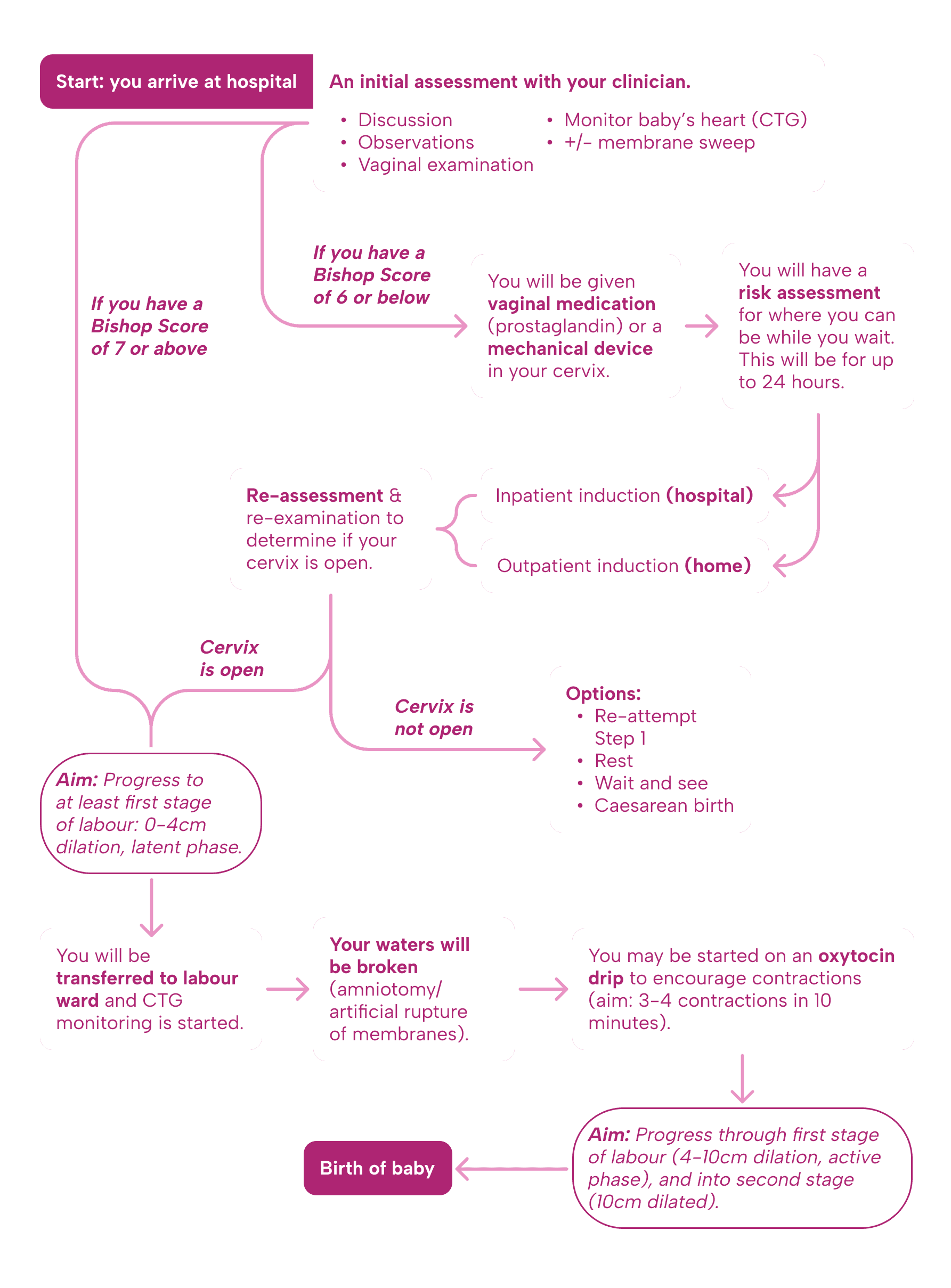
Each step, detailed
Your arrival for induction:
Induction of labour can be carried out in hospital (inpatient) or at home (outpatient).
Outpatient induction may be offered with vaginal medication (prostaglandin) or a mechanical device in the neck of your womb (cervix).
This can be offered to women who wish to return home, and who have no medical problems or additional risks.
The risks and benefits of returning home should be discussed and your decision should be respected.
A clinical assessment will be carried out of you and your baby before induction begins including; vaginal examination, measuring your vital signs and monitoring your baby’s heart rate.
A plan will be made with you by your team before you return home.
When you are home, contact your team in hospital if:
contractions begin.
Your waters break.
You have vaginal bleeding.
You have any other concerns, such as reduced fetal movements, severe pain or uterine contractions very close together.
If your vaginal medication or mechanical device falls out.
Your place for induction or birth may change if you wish for or are recommended:
Certain medications (e.g. a hormone drip) or pain relief (e.g. an epidural) AND/OR
Your baby’s heart rate needs monitoring continuously
These may not be available for home birth or in a midwife-led unit, talk to your team about your preferences.
The initial assessment:
Factors affecting whether induction leads to active labour:
There are multiple factors associated with the success of induction. One of the main factors is the assessment of the cervix using the bishop score.
The Bishop score:
The Bishop score is a number obtained by doing a vaginal examination, and is based on:
How many cm dilated you are.
Length (effacement) of the neck of your womb (cervix).
Position of the neck of your womb (cervix) in your vagina.
Consistency of the neck of your womb (cervix).
How far down the pelvis your baby’s head is (station).
A score of 8 or more generally indicates that the neck of your womb (cervix) is more ready for labour. It is used during a spontaneous labour and during induction.
Other factors:
If you’ve had a vaginal birth before, this increases the chance of your induction leading to active labour.
Your baby being a within a normal weight range and you being from 37 – 40 weeks (term) increases your chance of induction leading to active labour.
If you have a high BMI (more than 30) you are more likely to have a caesarean birth during induction than those will a BMI less than 30.
Your age and if you have any medical conditions can influence your chances of the induction leading to vaginal or caesarean birth, talk to your obstetric team about your individual circumstances.
Care during induction of labour:
Before induction: The position of the baby and your condition are checked before induction begins.
This will involve:
An examination of your tummy (abdomen).
Carrying an ultrasound scan to check the position of your baby to check if they are head down (correct position).
Checking your baby’s heart rate pattern using a machine called cardiotocography (HL).
Looking at whether you are contracting regularly or not.
Your team will offer you a vaginal examination to assess the readiness of the neck of your womb (cervix) to help to decide which method of induction to offer first. Vaginal examinations are needed before and during induction, to determine the best method of induction and to monitor progress in labour.
During induction:
When your Bishop score is 6 or less you will be offered: Vaginal medication, or Mechanical method (a balloon inserted into the neck of your womb).
When your Bishop score is more than 6, you will be offered: Breaking your waters (amniotomy) and giving a hormone (oxytocin) drip through a vein in your arm.
See more about options for starting labour and induction of labour here
Pain relief options are available during your induction.
Care during induction may differ. For example:
With vaginal medication; your baby’s heart rate and your contractions will be checked regularly.
You can develop excessive contractions (hyperstimulation) if this happens, your vaginal medication will be removed (if possible), or your hormone drip will be stopped. There is also medication that can slow your contractions down.
Induction with a mechanical device in the neck of your womb is less likely to cause excessive contractions than vaginal medication.
When uterine contractions begin:
The first stage of labour is 0-10cm dilatation of the neck of your womb (cervix)
If your contractions become regular and happen about 3 or 4 times in ten minutes, a vaginal examination is offered to you to check whether you are in active labour (4cm dilated or more).
The purpose of a vaginal examination is:
Check how thin and dilated your cervix is.
To see how far down your pelvis your baby’s head is lying.
See what position their head is in, in relation to your pelvis.
Check for any swelling on your baby’s head (caput).
Check your waters (membranes) before breaking them.
You can decline and ask to stop at any stage during the examination.(1)
Possible variations
Potential variation in length of induction of labour.
There is a potential variation in length of induction of labour depending on different ways in which you are induced and your body’s response.
Induction of labour varies but prepare to be in hospital for 2 days or more. There is currently no data available stating the average length of an induction of labour in the UK.
Step 1: Cervical ripening – takes up to 24 hours, it may be longer if more than one method is used.
Step 2: Getting into active labour to delivery:
First stage of labour (1-10cm dilated):
First labours last an average of 8 hours and are unlikely to last over 18 hours.
Second and subsequent labours last an average of 5 hours and are unlikely to last over 12 hours.
Breaking your waters and use of the hormone drip (oxytocin) may impact your length of labour.
Second stage of labour (10cm dilated to birth)
First labour without epidural: birth within 3 hours of active or involuntary pushing.
First labour with epidural: up to an additional 2 hours without pushing.
Second or subsequent labour without epidural: birth within 2 hours of active or involuntary pushing.
Second or subsequent labour with epidural: up to an additional 1 hour without pushing.
Depending on what type of birth you have (vaginal or caesarean) will impact on your postnatal length of hospital stay.
There will be management of the third stage of birth: the birth of the placenta and reducing bleeding after birth. Find more information about giving birth to the placenta here.
Induction urgency levels and its impact on the length of the process.
A pregnancy continuing after 41+0 weeks increases the likelihood of:
Unplanned caesarean birth
Baby needing admission to a neonatal intensive care unit
Stillbirth and neonatal death.
Induction of labour from 41+0 weeks may reduce these risks.
Induction during specific situations:
If your waters break at or after 37 weeks you can choose to:
Wait for up to 24 hours
Have induction of labour straight away
If you are known to have a bacteria called group B streptococcus in your vagina, you will be offered immediate induction of labour if your waters break any time from 34 weeks.
Information regarding partners, their presence and role during the birth:
Partner refers to the woman's chosen supporter. This could be the baby's father, the woman's partner, family member or friend, or anyone who the woman feels supported by and wishes to involve in her antenatal care.
Partners are welcome to attend antenatal appointments and classes for information.
Having a trusted birth partner present throughout labour is known to make a significant difference to the safety and well-being of women in childbirth.
Birth companions can:
Support information giving, receiving and general communication.
Advocate for the woman/birthing person.
Provide practical support, including encouraging women to move around, providing massage, and holding their hand.
Provide emotional support, using praise and reassurance to help women feel in control and confident, and being continuously present.
References:
National Institute for Health and Care Excellence: Guidelines. Inducing labour. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2021.; 2021.
Marconi AM, Bozzetti P, Morabito A, Pardi G. Comparing two dinoprostone agents for cervical ripening and induction of labor: a randomized trial. Eur J Obstet Gynecol Reprod Biol. 2008;138(2):135-40.
Batinelli L, Serafini A, Nante N, Petraglia F, Severi FM, Messina G. Induction of labour: clinical predictive factors for success and failure. J Obstet Gynaecol. 2018;38(3):352-8.
Parkes I, Kabiri D, Hants Y, Ezra Y. The indication for induction of labor impacts the risk of cesarean delivery. J Matern Fetal Neonatal Med. 2016;29(2):224-8.
Ellis JA, Brown CM, Barger B, Carlson NS. Influence of Maternal Obesity on Labor Induction: A Systematic Review and Meta-Analysis. J Midwifery Womens Health. 2019;64(1):55-67.
National Institute for Health and Care Excellence: Clinical Guidelines. Intrapartum care. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2023.; 2023.
National Institute for Health and Care Excellence: Guidelines. Antenatal care. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2021.; 2021.
Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7(7):Cd003766.
Bohren MA, Berger BO, Munthe-Kaas H, Tunçalp Ö. Perceptions and experiences of labour companionship: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;3(3):Cd012449.